Sustaining equitable Universal Health Coverage for key and vulnerable populations

UNAIDS joined the Asian Development Bank in January to hold a side meeting at the Prince Mahidol Award Conference (PMAC) on “Sustaining Equitable Universal Health Coverage for Key and Vulnerable Populations”. The meeting featured a panel of experts from government, civil society, ADB and UNAIDS and The participants explored the roles of government and development partners in ensuring adequate financing for Universal Health Coverage in the current era of poly-crises.
Universal Health Coverage (UHC) – one of the 2030 Sustainable Development Goals (SDGs)[1]– is about ensuring that all people receive quality health services they need without facing financial hardship. SDG target 3.8 is designed to “achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.”
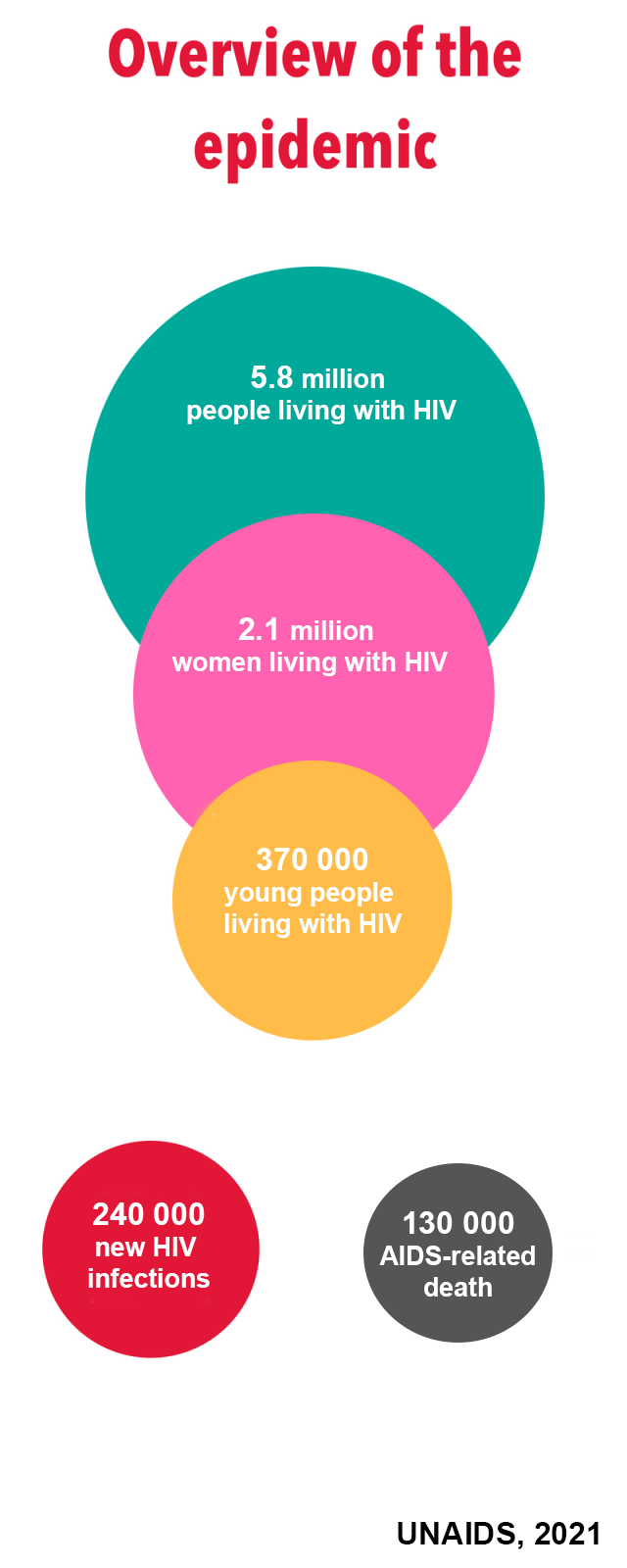
In his opening remarks, Mr Eamonn Murphy, Regional Director of UNAIDS, emphasized the importance of investing in UHC to build robust and resilient health systems in order to achieve gains across the SDG3 targets. This includes ending AIDS as a public health threat (SDG target 3.3).

“The effort to achieve Universal Health Coverage is intrinsically linked to the HIV epidemic. HIV investments are already making substantial contributions by expanding access to health services, helping countries strengthen their health systems, and laying the foundation to achieve and sustain universal health coverage,” Mr Murphy said. He noted the critical role of communities in the HIV response, especially in reaching key and vulnerable populations with essential health and HIV services, thus leaving no one behind.
Dr. Lo Veasnakiry, Secretary of State from the Ministry of Health of Cambodia, shared Cambodia’s remarkable experience in health financing as a critical component in achieving UHC by 2030 and strengthening a resilient health system. Cambodia increased its financial protection coverage for the poor and most vulnerable groups from 26% in 2019 to 36% of the total population in 2022 through the Health Equity Fund (HEF) and the National Social Security Fund (NSSF). HEF and NSSF led to more equitable access to, and increased utilization of, medical health services, reducing the amount of out-of-pocket spending on healthcare. Despite the progress made towards equitable health financing, Dr. Lo Veasnakiry stated that more needs to be done in the health sector to advance social health protection and expand healthcare services towards UHC.
The role of civil society was central to the discussion. Ms. Thissadee Sawangying, Director of the Health and Opportunity Network (HON), spoke about community leadership in the response to HIV. Reflecting on her work in providing HIV care and support services for transgender people living with HIV in Pattaya, Thailand, she emphasized the need to pay particular attention to the marginalized groups that bear the disproportionate burden of HIV, including men who have sex with men, female sex workers, and people who inject drugs.

She also mentioned other vulnerable groups as requiring care and support, including women and children affected by HIV, homeless and unemployed individuals, the elderly, and migrants. Ms. Sawangying spoke about long-term financing as an essential strategy to ensure sustainability of the response, and she called for enhanced support to communities from the Government, business, and other key sectors. She urged the Government to involve communities as key partners in planning and decision-making for health policies and programmes.
Dr. Eduardo Benzon, Principal Health Specialist at the Asian Development Bank (ADB), spoke on the role of multilateral financing in promoting UHC. He presented an overview of the ADB’s health strategy, health operations and areas of focus with targeted investments in gender equality, climate resilience, and pandemic preparedness and response. ADB provides financing, technical assistance, and knowledge solutions and services to accelerate progress toward UHC in Asia and the Pacific. ADB is making significant contributions to helping Asia and the Pacific become a more prosperous, inclusive, and resilient region.
The last presentation addressed the role of multilateral financing mechanisms in strengthening health systems. Evidence shows that progress in the HIV response is strongest where financial investments are highest. Dr. Jaime Atienza Azcona, Director, Equitable Financing from UNAIDS, pointed to ways to enhance investments for HIV programmes and health, leading to increased fiscal space for all sectors, prioritization of the health sector, efficient public financial management, and debt relief. He reiterated the benefits of HIV integration into UHC which would offer a cost-effective approach to enhance the accessibility and uptake of HIV services, especially by the most vulnerable and key populations.
 UNAIDS Asia-Pacific
UNAIDS Asia-Pacific