Asia-Pacific faces a dangerous financial squeeze that is undermining prevention and community support
GENEVA/BANGKOK, 26 November 2025—The AIDS response has suffered its most serious setback in decades, warns a new UNAIDS report released ahead of World AIDS Day (1 December). Overcoming Disruption, Transforming the AIDS Response details how a sharp fall in international funding is hitting low- and middle-income countries hardest and threatening to reverse hard-won gains.
Read More
WHO and UNAIDS convene partners to explore solutions to the Region’s HIV crisis
NADI, Fiji, 22 October 2025 — The World Health Organization (WHO) Regional Office for the Western Pacific and UNAIDS Asia-Pacific have convened a range of stakeholders here to confront the Region’s HIV crisis amid growing national epidemics. Held during the seventy-sixth session of the WHO Regional Committee for the Western Pacific and at the request of the Fiji Ministry of Health and Medical Services, today’s high-level event brought together ministers of health from the 38 countries and areas of the Western Pacific Region, as well as civil society and development partners, to seek solutions to accelerate progress on HIV prevention.
Read More
Overcoming disruption, transforming the AIDS response – World AIDS Day 2025
The theme of this year’s World AIDS Day is “Overcoming disruption, transforming the AIDS response.”
Read More
Several Asia Pacific countries must act fast to reverse growing epidemics
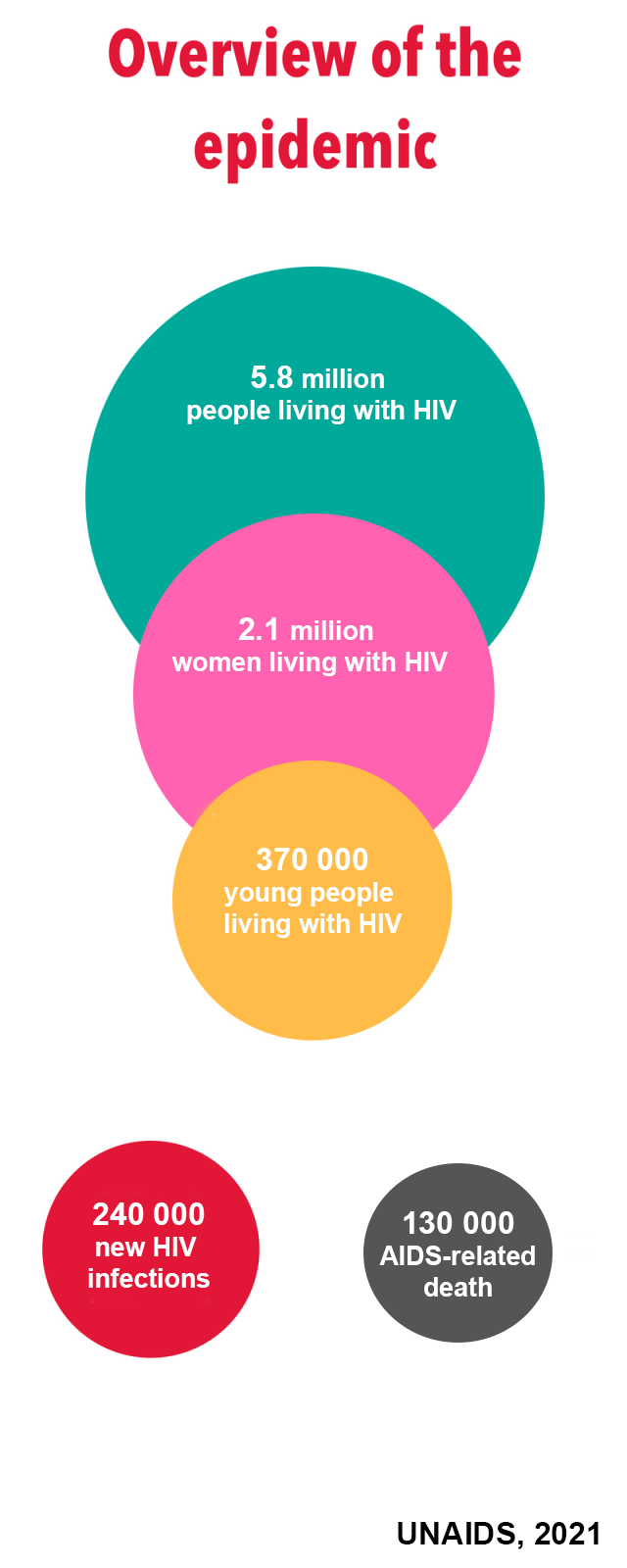
BANGKOK/GENEVA, 10 July 2025—Today UNAIDS launched its 2025 Global AIDS Update, “AIDS, Crisis and the Power to Transform”. It shows that a historic funding crisis is threatening to unravel decades of HIV response progress unless countries make radical programming and funding shifts.
Read More
This case study is featured in the 2025 Global AIDS Update
Kalesi Volatabu, founder of Drug Free World Fiji, breaks the ice at drug awareness sessions by sharing her shocking story.
Read More
PORT MORESBY, 26 June, 2025—New data reveal alarming rise in cases, particularly among women and children, with mother-to-child transmission rates critically high.
Read More
MANILA, 4 June, 2025–The Joint United Nations Programme on HIV/AIDS (UNAIDS) Philippines calls for immediate and intensified action to address the country’s rapidly escalating HIV epidemic, supporting the call of Department of Health for President Ferdinand Marcos Jr. to sign the pending Executive Order declaring HIV as an urgent public health concern requiring nationwide response.
Read More UNAIDS Asia-Pacific
UNAIDS Asia-Pacific