Regional Chemsex toolkit launched for clinical service providers

Partners explore more effective responses to sexualized drug-use at Asia Pacific Chemsex Symposium
BANGKOK, November 8, 2024—UNAIDS and the United Nations Office on Drugs and Crime (UNODC) have launched a first of its kind regional chemsex toolkit. Developed by the Australian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM), the toolkit is geared toward clinical service providers in Asia and the Pacific working with men who have sex with men and transgender women.
“Chemsex” refers to the use of stimulant drugs during sexual activity. This lowers inhibitions and may increase risk-taking. Its growing prevalence in the Asia Pacific region has several public health implications including higher rates of HIV and sexually transmitted infections (STIs), overdose and the fallout linked with intoxication.
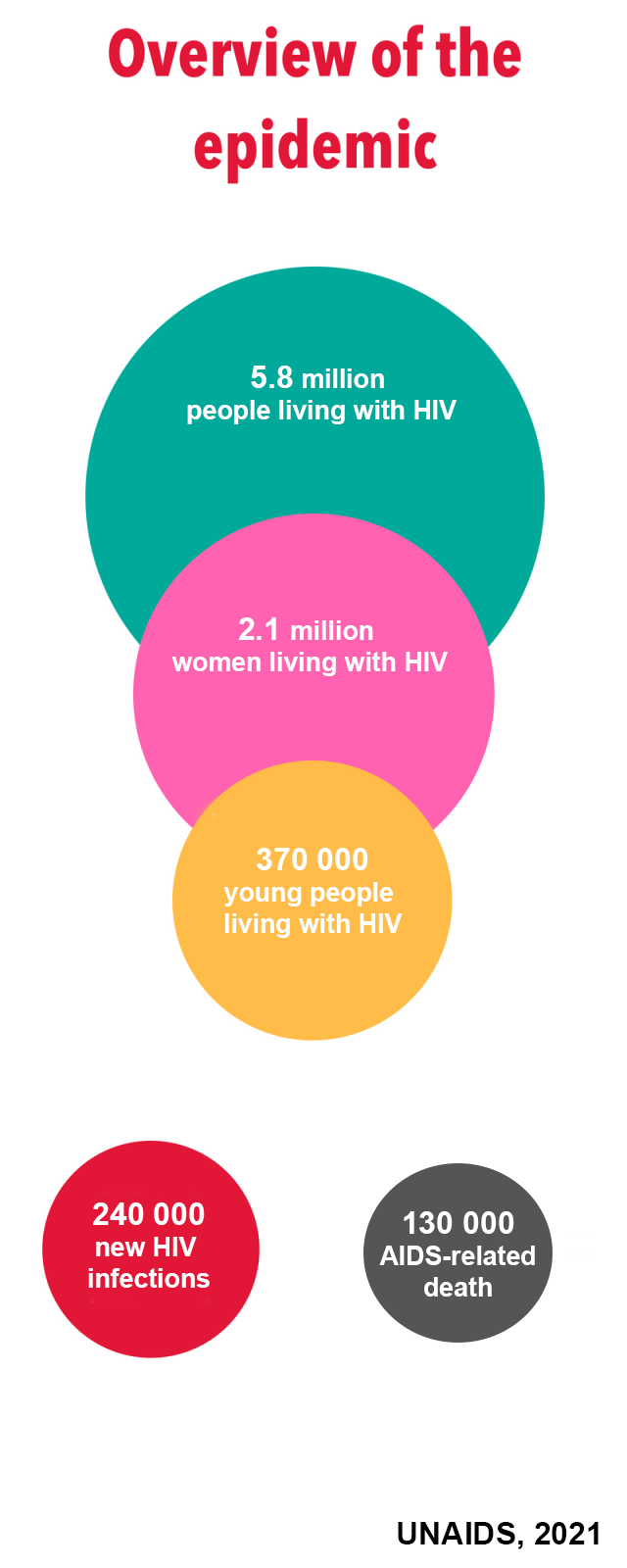
Four out of five new HIV infections in Asia and the Pacific occur in key populations, with about a quarter of new infections among young people aged 15-24. (Key populations are communities at higher risk for HIV infection, including men who have sex with men or MSM, people who use drugs, sex workers and transgender people.) The estimated prevalence of chemsex among men who have sex with men in Asian countries ranges from 3% to 31%, depending on the country. While chemsex is most visible in the MSM community, it is practiced by people from all populations.
“The work to respond to chemsex in our region is absolutely urgent for the HIV response,” said Eamonn Murphy, Regional Director of UNAIDS Asia Pacific and Eastern Europe Central Asia. “We need integrated sexual health and substance use services including access to HIV pre-exposure prophylaxis (PrEP), HIV testing, HIV treatment adherence support, regular screening for other STIs and harm reduction in a one-stop shop.” (PrEP is medicine taken by HIV negative people to avoid contracting the virus.)
“The increasing availability of stimulant drugs in the region and their use during sexual activity, or chemsex, poses significant health risks, including drug use disorders and various psychosocial challenges,” said Masood Karimipour, Regional Representative of UNODC’s Office for Southeast Asia and the Pacific. “This toolkit provides essential guidance for healthcare providers to address these challenges through evidence-based interventions. It emphasizes the importance of holistic, non-judgmental care that prioritizes the physical, psychological and social wellbeing of individuals, while ensuring access to harm reduction services and the prevention and treatment of drug use disorders within a comprehensive continuum of care.”
The toolkit was developed through consultation with clinicians, community representatives and government agencies. It outlines chemsex basics as well as approaches to harm reduction, sexual health and mental health services. It also covers different service delivery models including face-to-face, online and by communities. The toolkit offers guides on topics such as initiating non-judgmental conversations and risk assessment.

The Asia Pacific Chemsex Symposium
The toolkit was launched at the 6th Asia Pacific Chemsex Symposium (APCS), held in Bangkok from 6 to 7 November. Over 300 participants from 27 countries shared analysis and approaches to help stakeholders respond to the region’s growing practice of chemsex in an evidence-based way.
“This year’s theme is ‘pleasures, possibilities, policies’ emphasizing that we want to shift away from a risk-based approach which has proved to be not very effective, to a ‘pleasure-based approach’,” explained Dr. Nittaya Phanuphak, Executive Director of the Institute of HIV Research and Innovation (IHRI).
The APCS started in 2019 in Taiwan as a culturally sensitive and safe space for communities, researchers, healthcare professionals, policymakers and development partners to address this challenge. The symposium featured analysis of chemsex patterns in Asia-Pacific and gaps in healthcare and policy interventions. It also explored current intervention models, challenges, lessons learned and opportunities. Participants agreed to the following policy, research and service delivery recommendations:
- Most chemsex services should be designed and delivered by communities.
- Service packages that address chemsex should be comprehensive, including HIV and STIs, harm reduction, mental health, social, legal and human rights issues.
- Service offerings should offer clients various options and respect their agency to choose.
- More field work evidence is required to ascertain which interventions are feasible for scale-up, including pleasure-based approaches.
- Emphasising the right to health, deepened efforts are required to address the stigma, discrimination, laws and policies that undermine effective public health responses for key populations.
 UNAIDS Asia-Pacific
UNAIDS Asia-Pacific