PrEP for her

Cambodia, Indonesia, Papua New Guinea and the Philippines prepare to introduce the DVR
When Elena Felix contracted HIV the only prevention tools available were condoms. She didn’t think she needed them then. Thirty years after her diagnosis, she’s helped conduct research to determine whether women in the Philippines would use a new tool to lower their risk of HIV infection.
“It’s important for sex workers whose clients insist on not using condoms or might even rape them. It’s also an option for women whose partners might be injecting drugs or having sex with men,” the Association of Positive Women Advocates founder explained.

The Dapivirine Vaginal Ring or DVR was given the green light by the World Health Organization for women at high risk of contracting HIV in 2021. Unlike other types of pre-exposure prophylaxis (PrEP), this one is exclusively for women. It is a silicone vaginal ring that is inserted and worn for 28 days before being replaced. It releases an antiretroviral drug locally, reducing the risk of HIV infection through vaginal sex by half.
Since its introduction, the technology was made available in several African countries. And with good reason. Around two-thirds of new HIV infections in Eastern and southern Africa and Western and central Africa are among adolescent girls and women. The combination prevention strategies implemented in these two regions have super-charged progress, driving the global 39% decline in new infections since 2010.
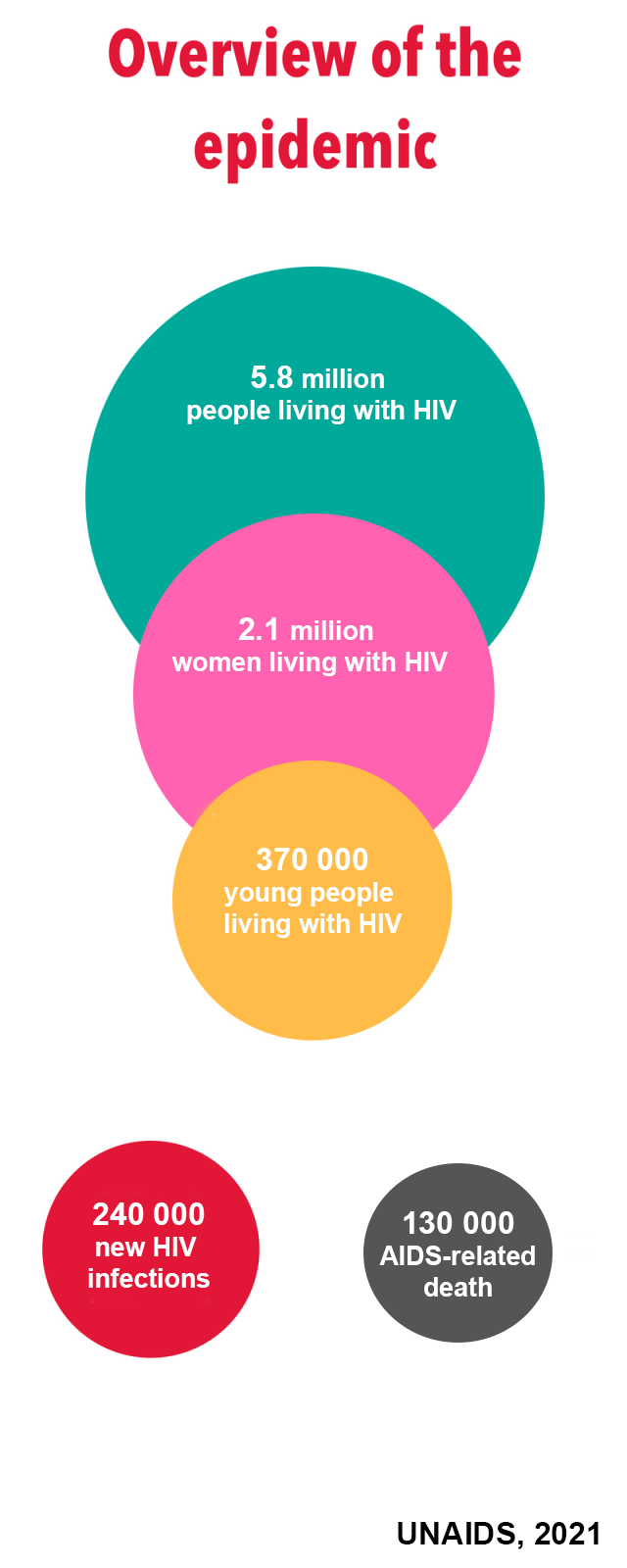
But the Asia Pacific picture is quite different.
“This region has an HIV prevention crisis,” Eamonn Murphy, UNAIDS Regional Director for Asia Pacific and Eastern Europe Central Asia said. “And I am not speaking only of the countries where new infections have doubled, tripled or increased six times since 2010. The average regional decline in new infections is far too slow. At 13% it has virtually flatlined.”
He was speaking to a group of community, government, research and development partners from Cambodia, Indonesia, Papua New Guinea and the Philippines who met from November 11 – 12 in Bangkok. They reviewed findings from a DVR acceptability and feasibility study conducted by ThinkPlace and decided on next steps. UNAIDS and the World Health Organization (WHO) are providing technical support for this initiative. The Australia Department of Foreign Affairs and Trade (DFAT) funded the research as part of its ongoing support for prevention work in the region.
Seven percent of new infections in Asia Pacific are among sex workers while 12 percent occur among the intimate partners of key populations. Angeli Achrekar, UNAIDS Deputy Executive Director, called for Asia Pacific women in need to have more HIV prevention options.
“Choice is the way to go!” Ms Achrekar stressed. “Providing options in prevention tools and service delivery increases overall use and results. We must ensure that people have access and that they are supported with the appropriate policies and enabling environment. The ring has great potential to be empowering as an additional choice for women in Asia Pacific.”
There is a new infection in the Asia Pacific region every two minutes. Despite this, the overall momentum on rolling out pre-exposure prophylaxis (PrEP) options has been sluggish. (PrEP refers to medicines used by HIV negative people to avoid contracting the virus.) At the end of 2023 there were just 204,000 PrEP users in this region, 98% short of the 8,200,000 target by 2025. The vast majority of those on PrEP were men.
ThinkPlace Regional Director, Elliot Duffy, revealed that overall, the studies found high interest in this discreet, woman-controlled prevention method. Sex workers in the four countries broadly accepted the DVR given their high vulnerability to sexual violence. And in all countries the sex workers indicated that they would be willing to access the DVR through community-based health services or their local healthcare facilities. The research also found that healthcare providers in the four countries were enthusiastic about offering this new prevention option.

“The number one barrier is the extent to which women understand their biology and how the ring would fit. Many had questions like, “would it be lost in my body? Will I feel pain? Will I be able to have sex?’ Some women worried about a partner thinking they distrusted them,” Mr Duffy explained. “The DVR is not immune to the challenges of other HIV programs and continued effort is needed to increase awareness, generate demand and create services that are accessible.”
Already the research findings have resulted in the introduction and phased implementation of the DVR into 2024 – 2026 Global Fund grant implementation for Cambodia and Indonesia. Cambodia has begun pilot testing. At the meeting the four country teams developed plans to guide their next steps, including on further research, legal and policy reviews, regulatory approvals and community system strengthening.
DFAT Health Adviser, Joshua Metcalf-Wallach, emphasized that as stakeholders switched gears from research to rollout, they should keep communities in the driver’s seat.
“Our Indo-Pacific prevention work has shown that HIV services work best when they are key population- and community-led. As we expand prevention options for women, let us be guided by their needs and demands,” he ended.
 UNAIDS Asia-Pacific
UNAIDS Asia-Pacific